Hypoparathyroidism Symptoms and Treatment Guide
Understanding Hypoparathyroidism
Hypoparathyroidism is a rare endocrine disorder characterized by an insufficient production of parathyroid hormone (PTH) by the parathyroid glands. These tiny glands, located near the thyroid in the neck, play a crucial role in maintaining calcium and phosphorus balance in the body. When PTH levels are low, it can lead to decreased calcium levels and increased phosphorus levels in the blood, resulting in a variety of symptoms that can impact nerve, muscle, and bone function.
Recognizing the importance of calcium in the body underscores why hypoparathyroidism matters. Calcium is vital for numerous physiological processes, including muscle contractions, nerve signaling, and bone health. A deficiency can cause a range of symptoms from mild tingling in the fingers to severe muscle cramps and seizures. In the long term, untreated hypoparathyroidism can lead to complications such as cataracts, dental issues, and calcification in the brain.
Hypoparathyroidism is most commonly caused by surgical removal or damage to the parathyroid glands during thyroid surgery. Other causes include autoimmune diseases, genetic conditions, or radiation treatment to the neck. Understanding these causes is essential for early diagnosis and effective management of the condition.
The Current Relevance of Hypoparathyroidism
In recent years, the prevalence and awareness of hypoparathyroidism have gained attention, especially in the United States, where post-surgical cases are most common. As surgical techniques improve and more people undergo thyroid and parathyroid surgeries, the incidence of hypoparathyroidism as a complication has become more pronounced. This highlights the need for improved surgical techniques and postoperative care to minimize risks.
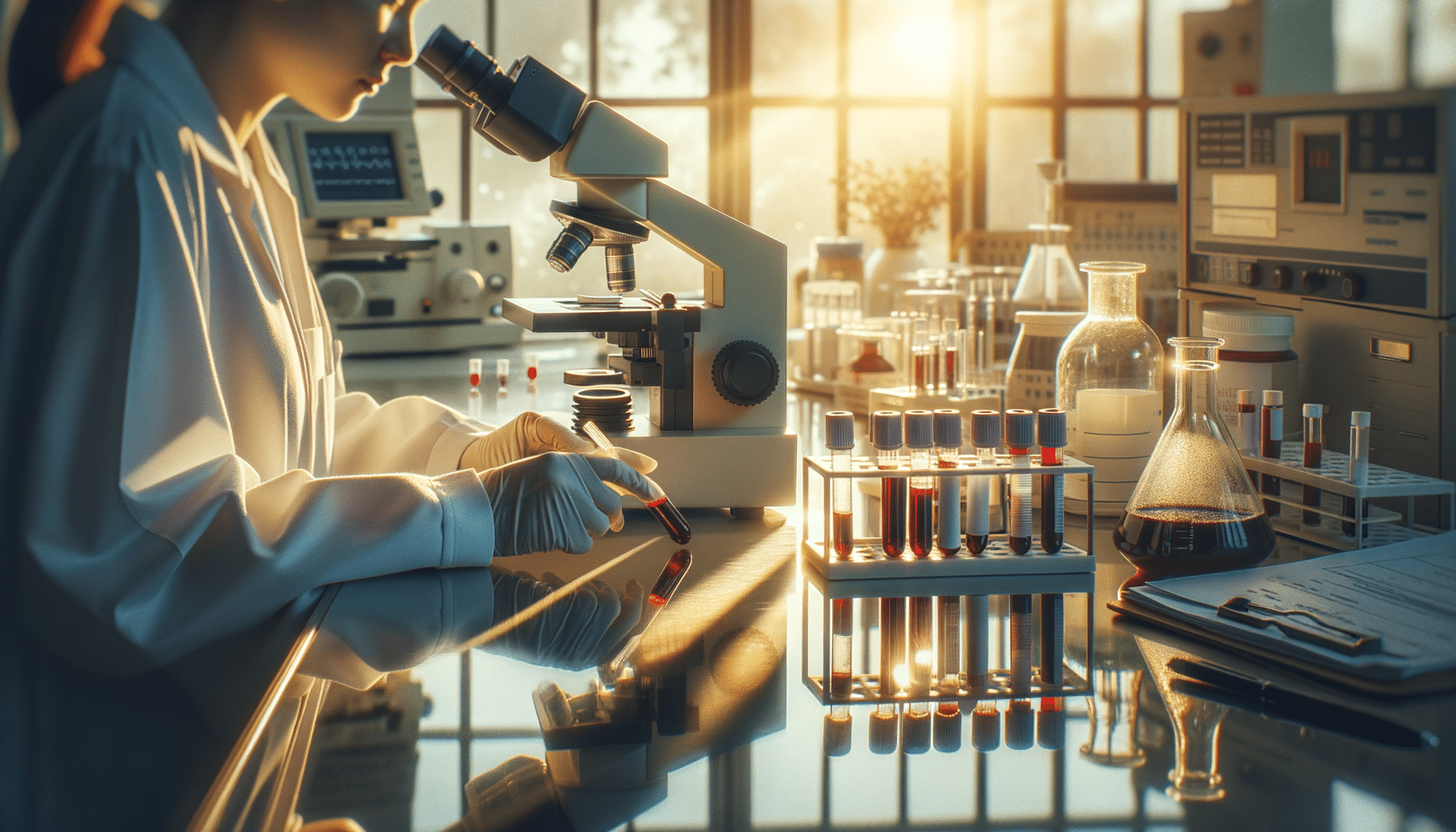
Moreover, advancements in diagnostic tools have made it easier to identify and confirm hypoparathyroidism, allowing for timely intervention. Blood tests measuring calcium, phosphorus, and PTH levels are critical in diagnosing the condition. Early recognition can prevent the progression of symptoms and reduce the risk of chronic complications.
The increased focus on hypoparathyroidism also reflects a broader trend in medicine towards personalized care. Understanding the unique needs of patients with this condition can lead to more tailored treatment plans, improving quality of life and reducing healthcare burdens.
Symptoms and Diagnosis
Hypoparathyroidism manifests through a variety of symptoms that can be acute or chronic. Common symptoms include:
- Tingling or burning sensations in the fingertips, toes, and lips
- Muscle cramps and spasms
- Fatigue and weakness
- Anxiety and mood changes
- Dry skin and brittle nails
- Seizures in severe cases
Diagnosing hypoparathyroidism involves a combination of clinical evaluation and laboratory tests. A detailed medical history and physical examination are the first steps. Blood tests are used to measure calcium, phosphorus, and PTH levels, confirming the presence of hypoparathyroidism. In some cases, imaging studies of the neck may be used to assess the parathyroid glands.
Early and accurate diagnosis is crucial, as it allows for prompt treatment and management of symptoms, preventing potential complications. Patients experiencing persistent symptoms should seek medical advice to explore the possibility of hypoparathyroidism.
Benefits of Effective Treatment
Treating hypoparathyroidism effectively can significantly improve a patient’s quality of life. The primary goal of treatment is to restore normal calcium and phosphorus levels in the blood. This is typically achieved through calcium and vitamin D supplements, which help manage symptoms and prevent complications.
In some cases, recombinant PTH therapy may be prescribed to patients who do not respond adequately to standard treatments. This therapy mimics the action of natural PTH, helping to regulate calcium levels more effectively. However, it is usually reserved for severe or refractory cases due to its cost and potential side effects.
Effective treatment can alleviate symptoms such as muscle cramps and fatigue, reduce the risk of long-term complications like cataracts and cardiac issues, and improve overall well-being. Patients who adhere to their treatment plans often experience a marked improvement in their daily lives.
Moreover, managing hypoparathyroidism effectively can reduce healthcare costs by decreasing the need for emergency care and hospitalizations related to acute symptoms or complications. This underscores the importance of regular follow-up appointments and monitoring to ensure optimal treatment outcomes.
Conclusion: Managing Hypoparathyroidism
For individuals living with hypoparathyroidism, understanding the condition and its implications is the first step towards effective management. With advances in medical research and treatment options, patients can lead healthier lives with fewer complications. Early diagnosis and adherence to treatment are key to managing symptoms and improving quality of life.
Healthcare providers play a crucial role in educating patients about their condition, helping them navigate treatment options, and providing ongoing support. By prioritizing patient-centered care, the medical community can continue to improve outcomes for those affected by hypoparathyroidism.
Overall, increased awareness and understanding of hypoparathyroidism are vital to ensuring that patients receive the care they need. As research continues to unfold, it is hoped that new therapies and management strategies will further enhance the lives of those living with this challenging condition.